When your surgery goes wrong hospitals profit The Washington Post
Post on: 16 Март, 2015 No Comment

By Sarah Kliff April 16, 2013
For a patient, a surgical complication can be a painful, even deadly. For a hospital, a surgical complication can be incredibly profitable.
A surgical complication increases a procedure’s average contribution margin by 330 percent for the privately insured and 190 percent for Medicare patients, according to a study published this week in the Journal of the American Medical Association.
The study underscores how ludicrous the incentives are in the American health care system, generally paying doctors for each medical service they provide, even if some of that care is the result of a surgery gone wrong.
If you personalize this and a relative is having heart surgery, which gets complicated by pneumonia, I don’t think we would want a hospital’s profit to go up as a result of that pneumonia, said study co-author Barry Rosenberg, a partner in Boston Consulting Group’s health care practice.
The study does not imply that hospitals intentionally complicate surgeries to bring in more revenue. Most surgeries, about 95 percent, go off without a hitch. What it does suggest to the surgeon, writer and Harvard professor Atul Gawande is that hospitals now see little reason to invest in technologies that would reduce complications when the only prize at the end would be lower income.
The JAMA study was born out of a joint project between the Boston Consulting Group and Gawande, who were trying to bring a safe surgery checklist into more hospitals.
Part of what we have been trying to unravel is why some of the simple quality control measures that we know work are very slow to penetrate, Gawande told me in an interview. This puts in perspective how weak the incentives are [to improve quality]. Complications produced massively higher profits.
Rosenberg explained, We started realizing that, if hospitals were to implement the safe surgery checklist and reduce complications that, paradoxically, hospital profits would fall.
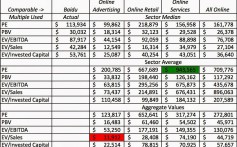
This study looked to quantify how much, exactly, a hospital had to lose if it reduced its number of surgical complications. It focused on claims data provided by a 12-hospital chain in the South. The hospital treated 35,394 patients for 12 common surgical procedures, including appendectomies and coronary artery bypass. Of those patients, 1,820 had complications ranging from an infection at the surgery site to cardiac arrest.
Patients who had complications had to spend more time in the hospital. They stayed for an average of 14 days in the hospital, compared to the three-day stays of surgical patients who experienced no glitches.
The surgical complications also generated tremendously higher contribution margins. This is the amount a hospital nets on a surgery after discounting all the costs devoted to the individual patients, such as the doctors or nurses who provided treatment. This does not include the cost of facilities or specific equipment but, as Princeton health policy economist Uwe Reinhardt writes in a commentary in the JAMA issue, this is a particularly good metric to measure a hospital’s long-term viability.
When a surgical complication occurred, the profit margin jumped from $16,936 to $55,953. For Medicare patients, profits grew from $1,880 to $3,269.
Most US hospitals treat patient populations primarily covered by Medicare or private payers and programs to reduce complications may worsen their near-term financial performance, the study’s authors contended.
What’s more, hospitals that do reduce complications don’t really get much of a reward at the end. The savings accrue to Medicare or private insurers who don’t have to pay out another claim.
Most of the value goes to the payer when most of the work is borne by the hospital, Rosenberg said.
To reset the incentives, Gawande and Rosenberg advocate taking more aggressive steps to tether doctors’ payments to the quality of care they provide. Right now, 90 percent of private market payments have nothing to do with value.
The additional money from complications is a lot of money to part with, unless what you’re doing is going to get rewarded, and you have a financial incentive to install a quality control program, Gawande said.
If hospitals receive a set amount for every heart surgery they perform, for example, they suddenly have an incentive to reduce complications — they know the extra medical spending will come out of their own budget.
Only 5.3 percent of patients have a complication, so we’re talking about 95 percent without that, Rosenberg said. It wouldn’t be crazy to think about paying a little bit more for the uncomplicated procedures, and the hospital bears some of the risk if something goes wrong.
Under that model, better results do translate into higher payments—the exact opposite of the system we have right now.