Getting Paid for Anesthesia Mastering the Challenges of Viability The Anesthesia Insider Blog
Post on: 3 Ноябрь, 2015 No Comment

Some of us are old enough to remember the days when anesthesia prtoviders got paid more or less based on what they decided to charge. It used to be that a favorable mix of patient insurance coverage (payor mix) and reasonably busy operating rooms was sufficient to ensure the financial viability of an anesthesia practice. There was a time when anesthesiologists talked about things like group formation, hospital contracts and managed care negotiations in the abstract as interesting options. Conventional wisdom held that a few persistent and disciplined secretaries would be sufficient to provide for the business requirements of the typical practice. Sadly those days of entrepreneurial opportunity have given way to a whole new set of practice management challenges. Survival and success now have much less to do with the favorability of the payor mix or even with the clinical qualifications of the providers; today’s practices must constantly monitor and manage an ever more complex balance sheet of income and expenses just to retain the opportunity to provide care. While practices in the 1980s were preoccupied with the arcane rules of concurrency and those in the 1990s worried about running afoul of HIPAA, today’s anesthesia practices have become consumed by a much broader and more complex set of business issues.
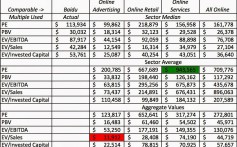
The reference data for this article were derived from a random sample of seven actual anesthesia practices all of which have experienced flat or declining revenue over the past three years. This is not intended as a statistical analysis of revenue patterns, but rather a conceptual review of the significant factors that affect the ability of moderate sized anesthesia practices to remain financially viable in today’s health care environment. Table 1 on this page provides a summary of three years of total practice income, including insurance payments, patient payments and hospital subsidies.
No fewer than five separate and distinct developments have dramatically reshaped the anesthesia landscape over the past decade and the rate of change appears to be speeding up. Success in anesthesia used to be like real estate: the only three things that mattered were location, location and location. A favorable practice setting used to be the only important pre-requisite but such is no longer the case. While location can still provide a competitive edge, it has become just one factor in a much more complicated financial proposition.
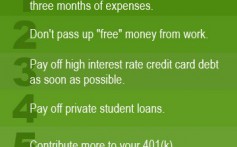
Consider how anesthesia providers get paid. It is no longer enough to simply send out claim forms to insurers to ensure adequate cash flow. It is back to the future of health care; good health care coverage is no longer affordable nor adequate to cover the costs of today’s anesthesia bills. The hot topic of the day is patient responsibility. And the challenge involves getting patients to pay their fair share. Aggressive managed care contracting is starting to create some serious obstacles and is greatly constraining the typical practice’s ability to realize overall increases in practice revenue.
Table 2 (below) shows the percentage of total practice revenues that have been paid directly by patients, either in the form of deductibles or co-payments or because the patients had no insurance. Percentages appear to be going down for most of the practices in this random sample, but this is simply due to the fact that commercial insurance and Medicare rates have gone up over this three year period, as have hospital subsidies. What the table underscores, however, is the challenge created when these other sources of revenue cease to increase.
The evolution of the accounts receivable management industry over the past couple of decades has seen an increased focus on technology and labor intensive approaches to revenue maximization. Software development has provided many options for submitting accurate claims as expeditiously as possible and powerful tools intended to confirm the accuracy of payments. These developments have moved us far from the early days of dialing for dollars to resolve outstanding patient accounts. Large billing companies now employ predictive dialers to leverage the productivity of the follow-up team but the fact remains that collecting balances from patients who may have neither the motivation nor the ability to pay for their share of health care is proving to be one of today’s greatest management issues.
In addition to the obstacles of getting paid for professional services rendered, too many anesthesia practices are now finding themselves caught in another squeeze play involving unrealistic coverage expectations on the part of hospital administrators. This unfortunate development has shed light on the other side of the anesthesia practice ledger: the cost of providing the care. The basic problem is simple: when hospitals ask for more coverage, the same revenue inevitably gets spread over more anesthetizing locations. It is a curious irony that the idea of making a hospital a more attractive place for surgeons to bring their patients has exactly the opposite effect on the anesthesia group. It is the rare practice that does not feel the effects of this squeeze play to some extent and many complain that they are constantly fighting Administration’s desire to add more coverage. Few practices have yet to develop an effective strategy to reset and manage administration expectations.
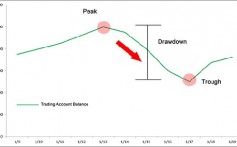
There are various methods used to evaluate operating room utilization, but anesthesia has a distinct advantage based on its ability to track actual cases, units and minutes billed per anesthetizing location. Historically, 50 ASA units billed per anesthetizing location per day was considered optimum productivity. This should equate to approximately 7 hours of billable anesthesia time. From a financial perspective most observers would agree that a reasonable target is $2,000 of gross professional fee income per location per day: this should be sufficient to compensate a physician working in a physician-only practice at the MGMA median compensation level. Staffing models based on the medical direction of CRNAs can generally reduce this revenue requirement but there are obviously a variety of factors that must be taken into consideration.
While many anesthesiologists feel helpless to stem the tide of declining operating room productivity, there are glimmers of hope across the landscape. Some of the nation’s largest hospital organizations have come to identify the improvement of operating room productivity as a key strategic objective. This does not diminish the importance of attracting more surgical cases but does tend to provide some hope that an objective allocation of operating room resources and staff might be achieved. In the meantime, anesthesia practices are having to develop an entirely new set of reporting and management tools to both monitor the appropriateness of operating room utilization and help hospital administrations reset surgeon expectations.
While the most logical and proactive approach would involve a concerted effort to educate the administration with relevant data and benchmarks, few practices have made the commitment to capture the necessary utilization data. Those that have, however, can attest to the value of the investment. The most creative have even used their utilization data as the basis for creative hospital subsidy arrangements that align the incentives of the hospital and that of the anesthesia group.
The third development is directly related to the second but it has become as much a philosophical as a financial challenge. Once fiercely independent anesthesia practices are being forced to open their books in order to obtain necessary financial support from their host hospitals. The revenue a practice can generate through its billing and collections activities is becoming less important than what they can negotiate as part of their exclusive contractual relationships. We have reached a point where it is not uncommon for a practice to receive 35% of total practice revenues in the form of hospital subsidy support. See Table 3.
Private anesthesia practices have evolved a culture that is specific and idiosyncratic to the specialty. Independence has been the hallmark of practice management strategy. Anesthesia practices have prided themselves on their ability to benefit symbiotically from their contractual relationships with hospitals. As is so often the case, however, the beliefs and strategies that got us to where we are today will not get us to where we need to be tomorrow. Nondisclosure of practice finances is proving to be a significant obstacle to fair and reasonable coverage agreements. Many hospitals have even started insisting on the right to review individual provider W2s. The reality is that there are fewer and fewer exceptional anesthesia practices from a financial perspective; rather there are those that are fairly compensated based on national benchmark data and those that need support. The hospital contract is becoming a form of specialty safety net.
As if these developments were not enough, the entire context of the anesthesia service is starting to be viewed in an entirely new light. Anesthesia providers used to thrive in the rarefied air of the operating room where their ability to make split second decisions ensured their value to the larger medical community. Little by little something changed and it was not enough to have consistently predictable outcomes. A new vocabulary of customer service has changed the nature of the service equation. Anesthesia is expected to support the overall business plan and mission of the institution. Problem providers have become the bane of the anesthesia group during hospital contract negotiations.
Much as group practices try to leverage their years of experience with administration and their ability to work with the surgical staff, they are being challenged by outside entities that purport to offer more services that will better support the hospital’s business plan. Whether the advantages of these national services are real or illusory seems to be of little relevance. As in so many things, new and improved seems to be more appealing than tried and true. Much as many practices do not want to admit it, the typical anesthesia franchise has become an object of considerable competitive value.
As if these developments were not enough, along comes healthcare reform. One more time federal policy is changing the rules of engagement and inspiring yet another wave of restructuring. Today’s vocabulary is distinctly reminiscent of that of managed care; Accountable Care Organizations (ACOs) appear to be the reincarnation of vertically integrated delivery systems. (See article on ACOs beginning on page 1.) Instead of paying individual providers on a fee for service basis, monies are allocated for the management of patient conditions. The more effective the management plan, the greater the profit potential for the provider.
ACOs and healthcare reform are still inchoate concepts but they are having a profound impact on the planning process. Like the high school students at the dance, the various players in the healthcare arena are starting to size each other up as they weigh their affiliation options. It is impossible to predict how this will all play out but one thing is quite clear, when it comes to health care there is no limit to the potential for complication.
These new realities are leading to the development of considerably different infrastructure and business decision-making requirements. Survival and success are no longer simply a matter of maximizing collections; but rather a function of a more global and comprehensive mastery of the entire practice balance sheet. It is no longer enough to just have a billing office or service, now practices find they need a full range of practice management services. These are boom times for consultants and administrators as it becomes ever clearer that the key to success has less to do with clinical efficacy and more to do with financial acumen.
Many an anesthesiologist or CRNA may long for the good old days when it was enough to work hard and focus on consistent clinical outcomes, but this would be little more than wishful thinking. Too many of the variables have been changed; nothing can be taken for granted. Every aspect of the anesthesia business proposition is in a state of transition. Anesthesia practices must now come to terms with entirely new revenue challenges and options. These options are no longer just about enhancing physician compensation, but rather a complex financial calculus to ensure the availability of qualified staff to meet customer expectations. Physicians who have spent their careers mastering arcane clinical protocols must now learn how to market their services and negotiate reasonable terms of compensation. As these developments are unfolding, government oversight and management continues to impose an entirely new set of rules on provider groups. These challenges have greatly increased the financial risks for the typical practice and traditional group practices are being displaced with increasing frequency by national management companies. Few practices are completely prepared for the new realities of healthcare, but most have the necessary prerequisites. Those who are willing and able to make the commitment, clarify the focus and implement effective strategieswill certainly be players. Outdated beliefs and strategies must be replaced with new ideas. As Lee Iacocca once said: The time has come to lead, follow or get out of the way.